What Is a Retinal Tear? The 5 Most Frequently Asked Questions
A retinal tear occurs when an opening develops in the back layer of the eye, preventing light from being properly perceived. It often presents with symptoms such as sudden flashes of light, floating spots, or a gray curtain-like shadow in the field of vision. If not detected early, a retinal tear can progress to retinal detachment and may lead to permanent vision loss.

A retinal tear is an eye condition that can lead to serious vision loss if it is not detected early. In this article, we answer the questions patients ask most often and provide reliable, clear information about the treatment process, recovery period, and important points to watch for.
What is a retinal tear?
The retina is a light-sensitive layer lining the back inner wall of the eye and plays a fundamental role in vision. A retinal tear occurs when this delicate layer develops a break or tear, or begins to separate from its normal position within the eye. These tears typically develop in areas where the retinal tissue has become weakened.
Retinal tears often present with symptoms such as sudden flashes of light (photopsia), floating spots or strands (floaters), or the sensation of a dark curtain in the field of vision. However, in some cases they may progress without noticeable symptoms. For this reason, regular eye examinations are especially important for individuals in high-risk groups.
Because retinal tears can be a precursor to retinal detachment (complete separation of the retina), early diagnosis and timely intervention play a critical role in preserving vision. At this stage, treatments such as laser photocoagulation can help prevent progression.
Can a retinal tear heal on its own?
A retinal tear consists of small openings or breaks in the retinal layer at the back of the eye. It commonly occurs due to age-related vitreous changes, trauma, or structural factors such as high myopia. If left untreated, a retinal tear may progress to retinal detachment, which can result in severe and permanent vision loss.
So, can a retinal tear heal on its own? Unfortunately, no. Retinal tears do not close spontaneously and may worsen over time, leading to more serious complications. Early diagnosis is therefore essential for protecting vision.
A retinal tear should always be evaluated promptly because:
- The retina does not have the ability to repair itself, so untreated tears may progress.
- Symptoms such as flashes of light, sudden floaters, or shadowing in the visual field may indicate a retinal tear.
- Early intervention (for example, laser photocoagulation) can prevent retinal detachment.
A retinal tear that goes unnoticed can eventually lead to significant vision problems.

Is face-down positioning required after retinal surgery?
After vitrectomy surgery for a retinal tear—especially if a gas bubble has been placed inside the eye—patients are often advised to maintain a face-down position. The main purpose of this positioning is to allow the gas bubble to press against the tear, helping it seal properly and supporting the healing process.
Why is face-down positioning important?
- Positioning of the gas bubble: The gas naturally rises due to gravity. When the patient lies face-down, the bubble presses directly against the torn area of the retina, aiding healing.
- Stabilizing the retina: Proper positioning helps the retina remain in place and reduces the risk of detachment.
How long is face-down positioning necessary?
The duration varies depending on the individual and the specifics of the procedure. The first few days are usually critical. In some cases, patients may need to maintain this position for several weeks, for most of the day. The exact plan is determined individually by the treating physician, taking the patient’s comfort and daily life into account.
Failing to follow positioning instructions, applying them incompletely, or stopping too early can reduce the effectiveness of treatment. Therefore, the postoperative period is a sensitive phase that requires strict adherence to medical advice.
Are retinal diseases genetic?
Retinal diseases affect the light-sensitive nerve layer at the back of the eye and can significantly impair vision. Are these conditions genetic? Some retinal diseases do have a hereditary component. Individuals with a family history of similar eye conditions may have a higher risk.
Genetic factors
Genetic factors can play an important role in the development of certain retinal diseases. Conditions such as retinitis pigmentosa and congenital retinal dystrophies are directly inherited, while problems like retinal tears may also be more common in families with similar histories—particularly among individuals with high myopia.
What should people with a family history pay attention to?
If retinal disease has been diagnosed in family members, this should not be overlooked. Early detection can slow or prevent progression in some conditions. Therefore:
- Routine eye examinations should not be neglected.
- Eye exams should be performed even in the absence of symptoms.
- Sudden flashes of light, new floaters, or a curtain-like shadow in vision should prompt immediate consultation with an eye specialist.
While genetic predisposition can increase risk, it does not guarantee that a disease will develop. Conditions such as retinal tears are often preventable and treatable when detected early. Regular monitoring is key.
What are the treatment options for retinal tears?
A retinal tear is an urgent eye condition that can threaten vision. It often develops after posterior vitreous detachment and, if not treated early, may progress to retinal detachment and permanent vision loss. Fortunately, modern medical advances allow for prompt and effective treatment.
1. Laser treatment
One of the primary treatments for a retinal tear is laser photocoagulation. In this procedure, small laser burns are applied around the tear to seal the retina in place. This helps prevent enlargement of the tear and stops fluid from passing underneath and causing detachment.
- Advantage: Generally painless, usually does not require anesthesia, and can be performed on an outpatient basis.
2. Surgical treatment
If the retinal tear has progressed and detachment has occurred, surgical intervention may be required. Common methods include:
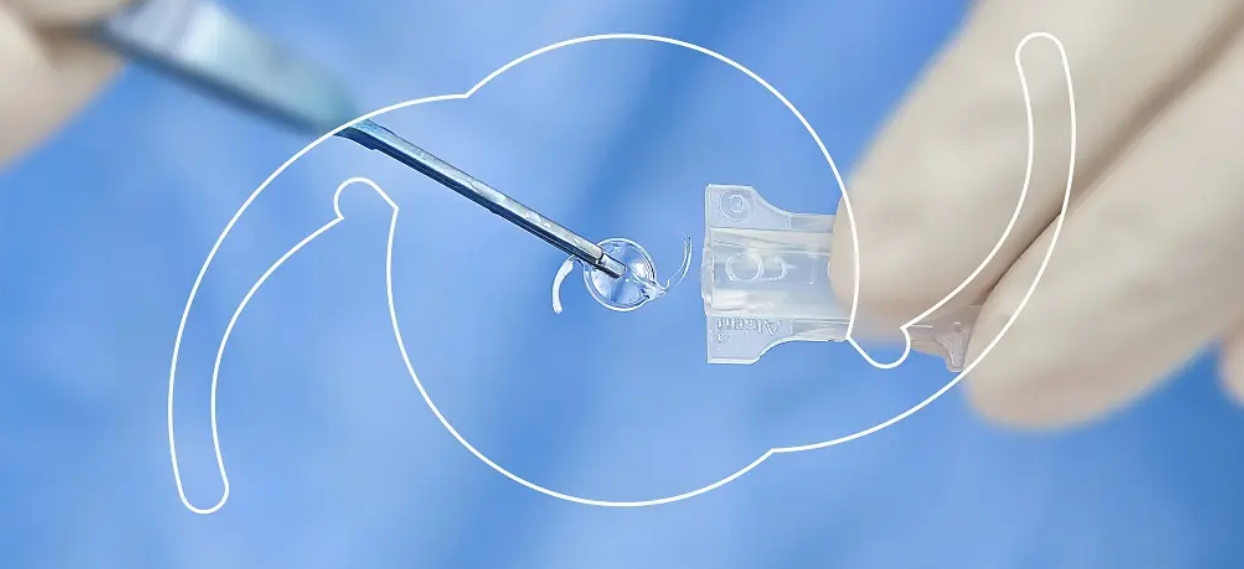
- Pneumatic retinopexy: A gas bubble is injected into the eye. With specific head positioning, the bubble presses the retina back into place, followed by laser or cryotherapy.
- Scleral buckle surgery: A silicone band is placed on the outside of the eye to help the retina reattach to the eye wall.
- Vitrectomy: The vitreous gel inside the eye is removed, allowing the retina to be repositioned. Gas or silicone oil may be used if necessary.
Post-treatment follow-up
Regular follow-up is essential after any treatment. A treated retinal tear may recur, or similar problems may develop in the other eye. For this reason, ongoing monitoring is just as important as the treatment itself.